A nutritional assessment is a comprehensive evaluation done typically by nutritionists or trained health professionals to define an individual’s overall nutrition status by determining whether their body is receiving the necessary nutrients. It can be done in home-based care, in a health care facility, or during support group conferences. While the assessment is mostly conducted on malnourished patients or those at risk of malnourishment, anyone who wants to know their health status and how to improve their nutritional choices can visit a nutritionist on the same. Understanding how the food they eat relates both positively and negatively to their health will encourage them to eat more nutritious foods. A nutritional assessment involves taking;
- Anthropometric Measurements.
- Biochemical Assessments.
- Clinical Assessments.
- Dietary Assessments.
Anthropometric Measurements
Anthropometric measurements are the measures of physical dimensions of height and weight, and proportions of the body.
Measuring Height
The heights of adults and infants alike can be measured using a stadiometer, height board, length board, or measuring tapes. On its own, an individual’s height does not particularly indicate their health. However, combining their height and weight can tell much about their health. Normally, taller people typically weigh more compared to shorter people, hence the need to take into consideration the proportions of the measurements.

Procedure for measuring height/ length
- Remove the patient’s shoes, caps, or any bulky clothing.
- Ensure the stadiometer is perpendicular to the wall and the length board is laid flat on the floor.
- Have the person stand straight against the stadiometer with their legs straight and heels together, arms at the sides and shoulders relaxed, facing straight ahead.
- The back of the head, shoulders, buttocks, back of legs, and heels should touch the vertical surface of the height board.
- Place the sliding headpiece down to touch the head and take the readings with your eyes parallel to the headpiece to avoid any errors.
- For greater accuracy, take the measurements twice and calculate the average.
- Record the height to the nearest 0.1 cm.
NB:
If the person cannot stand on their own, measure their recumbent length and subtract 0.7 cm to convert it to height.
Weight
An individual’s weight is usually strongly connected to their health status. Unintentional loss of weight can indicate poor health and the body’s inability to fight off infection. Gaining weight can be an indicator of poor nutritional practices or if the person is under certain medications, a side effect of the same. Low pre-pregnancy weight and too little weight gain during pregnancy are both indicative of growth problems and potential low birth weight for babies. For adults, a scale is used to measure weight while for newborns, digital scales or a balance beam are used.
Procedure for measuring weight
- Calibrate the scales before the subject steps on them.
- Ask the subject to remove any heavy clothing or accessories and to remain calm.
- Note the subject’s state and the testing time to ascertain any future tests can be done under similar conditions (check their state of hydration and the kind of food consumed recently).
- Take the readings from the front with the subject facing straight ahead and standing still on the scales.
- Wait for the digital screen/ pointer to settle and record the measurement.
- Repeat the measurements and calculate the average for greater accuracy.
- Record the measurement to the nearest 0.1 kg.
Body Mass Index (BMI)
BMI is a measure of an individual’s body fat based on comparing their weight against their height. It is very common when measuring body weight as a risk factor for cardiovascular disease and diabetes. It applies equally to both men and women. BMI is calculated using the following formula;
BMI = weight (kg)/Height (m)2
The BMI score is derived using a BMI chart as shown below;
BMI Categories
Underweight = <18.5
Normal = 18.5-24.9
Overweight = 25.0-29.9
Obesity = 30.0->40
Mid Upper Arm Circumference (MUAC)
Mid-upper-arm circumference (MUAC) is the measurement of arm muscle and fat area. It measures the circumference of the mid-upper arm at the mid-point between the tip of the elbow and the tip of the shoulder. In severely malnourished people, MUAC identifies the individuals at risk of mortality and those with morbidity. To measure MUAC, a MUAC measuring tape that shows millimeter measurements is used. MUAC assessments are done to measure the nutrient reserves in fat and muscle. The measurement is normally taken on the left arm as it is less active.
Procedure for measuring MUAC
- The subject should be seated and relaxed with their left arm bare.
- Locate the acromion (the tip of their shoulder) and the olecranon (point of their elbow).
- Measure the distance between the two points and mark the midpoint on the arm.
- Ask the subject to hang their arm loose and measure the circumference of the arm at the midpoint using a MUAC tape or a tape measure. The tape measure should fit comfortably around the circumference of the arm; not too tight nor too loose.
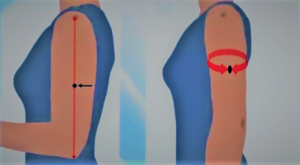
- Read the tape measure to the nearest 0.1cm.
- Measure the mid-upper arm circumference thrice.
- Record all three measurements and calculate the mean by adding all the values together and dividing by three.
Biochemical Assessment
A biochemical assessment tests for the nutrient and chemical levels present in the urine, stool, or blood. Healthcare professionals can use the test results to determine the subject’s health, any potential medical risks, or any medical problems they might have. The tests also measure the function of vital body organs like kidneys and liver. Below are some examples of biochemical measurements;
- Hemoglobin – Looks at the iron levels in the blood and indicates anemia.
- Albumin – At low levels, this can indicate infection or inflammation.
- C-reactive protein – Is an indicator of potential infection and inflammation.
- White cell count– Indicates an active immune system. A high white cell count indicates the presence of an infection.
- Glycated Haemoglobin – Is an indicator of an average blood sugar level for a period of months.
- Sodium Levels – Indicate the kidney function and hydration status. High sodium levels indicate dehydration.
- Urea Levels – Indicate kidney function and may demonstrate possible dehydration.
- Calcium and Phosphate Levels – Assess the risk of refeeding syndrome; a result of malnourishment.
- Magnesium Levels – Low levels indicate gastrointestinal losses.
- Micronutrients – Are impacted in the presence of an inflammation or infection.
Clinical Assessment
A clinical assessment identifies any diseases or health problems a person has that might affect their nutritional state or put them at risk of malnutrition. Diseases may cause a reduced intake of energy, an increased need for energy, or nutritional losses. Some of the diseases which may cause these changes are;
- Cancer
- Heart failure
- Chronic obstructive pulmonary disease.
- Gastrointestinal disorders such as Crohn’s disease, coeliac disease, liver disease).
- Burns, surgery, or trauma.
- Neurological conditions such as dementia, stroke, Parkinson’s disease, motor neuron disease, and multiple sclerosis.
- Mental health conditions like anxiety and depression.
Additionally, constipation, diarrhea, acid reflux, bloating, lethargy, nausea, vomiting, and difficulty in swallowing all signify an illness that may result in decreased nutrient intake or increased nutritional losses. Certain medications might have interactions with the individual’s digestion, absorption of nutrients, and metabolism. Nutritional deficiencies are also tested during a clinical assessment as they affect the effectiveness of medications. During a clinical assessment, the healthcare professional checks for signs of nutritional deficiencies which may include hair loss, changes in hair color, emaciation, and bilateral pitting edema (also known as nutritional edema).
Dietary Assessment
A dietary assessment provides information on the quantity and quality of food an individual eats and any changes in appetite, food intolerances or allergies, and times where they took inadequate amounts of food during or after an illness. It is essential in understanding nutritional health as it identifies the food and fluids one is consuming every day. Below are some of the methods used in conducting a dietary assessment;
- 24-hour Recall – This is when a patient recalls all of the foods and fluids they ingested in the last 24 hours. Patients recall the time they ate, and the size of their portions and this can be taken many times on different days, to record the day-to-day differences in eating habits.
- Food Frequency Questionnaire – This asks patients about the frequency of eating, the quality, and the quantity of the food they eat.
- Food Group Questionnaire – A healthcare professional shows visuals of various types of food and food groups to the patient and asks them whether they ate any of that the day before.
- Food Security Assessment – Involves assessing the patient’s physical and economic access to enough food to meet their nutritional needs. If they are struggling with food security, there are various support systems in place to help them have access to plentiful healthy food.
Supporting patients with their nutritional needs is very important as it helps them meet the daily requirements for healthy living. They might need assistance with functional aspects of nutrition. Since nutritional assessment is mostly done on malnourished patients or those at risk of malnourishment, the right knowledge and understanding are required to administer good nutrition and diet to millions of people across the world who suffer from malnutrition. Undertaking our professional training in Human Nutrition and Dietetics gives you an in-depth understanding and knowledge in nutrition and dietetics, which is critical in advancing your career.








(2) Comments